Causes and Treatments for a Broken Ankle

A broken ankle, involving a fracture of the bones in the lower leg above the foot, can result from various stresses on the ankle joint, often due to accidents or injuries. This may include rolling the ankle, twisting it, or sustaining significant force, such as landing heavily from a height. Determining whether the ankle is sprained or broken can be challenging, as both can be painful. Common signs of an ankle injury or fracture include pain, swelling, bruising, and deformity. A broken ankle is typically very painful, especially when bearing weight. Treatment for a broken ankle varies based on the type and severity of the fracture. It often involves immobilization using a boot or cast to allow for healing, along with non-weight bearing using crutches. More severe cases may require surgical intervention. After immobilization, the ankle can be left weak, stiff, and still painful. Exercises will then be needed to aid full recovery. If you suspect a broken ankle, it is suggested that you make an appointment with a podiatrist for a proper diagnosis and treatment.
Broken ankles need immediate treatment. If you are seeking treatment, contact one of our podiatrists from William Street Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact one of our offices located in William Street in New York, NY, Forest Hills, NY, and Broadway in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Broken Ankle Causes, Differences, Symptoms and Treatments
The ankle is a hinged synovial joint made up of three bones: the tibia (shin bone), the fibula (outer ankle bone), and the talus (between the heel and leg). These three bones are bound, supported, and stabilized by strong, fibrous bands of tissue called ligaments.
A break in an ankle bone can be either traumatic or stress related. This injury may be referred to as a break or fracture. A traumatic fracture can result from tripping, twisting or rolling the ankle, falling, or by blunt impact to the ankle. These traumatic ankle breaks usually occur during sporting activities or accidents. Stress fractures, however, occur over time and are the result of repetitive stress to the ankle. These fractures sometimes occur when a new activity that engages the ankle is introduced, or when the level of activity is abruptly increased or intensified.
There are various symptoms that accompany an ankle break. The most significant symptoms are pain and swelling that occurs in the ankle and sometimes spreads up from the foot to below the knee. Bruising or discoloration may develop eventually. It will be difficult or even impossible to put weight on the affected foot, and in severe cases there may be a visible deformity or even exposed bone.
It is very important to seek immediate treatment when an ankle break occurs or is suspected to have occurred, in order to allow the bone to properly heal and to avoid future complications such as stiff joints, limited range of motion, and osteoarthritis.
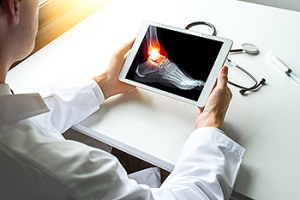
To diagnose a broken ankle, your podiatrist will first ask you to explain how the injury occurred and what your symptoms are. They will perform a thorough examination, checking for damage to nerves, blood vessels, and other structures around the injury site. They will also test your range of motion. An X-ray will need to be reviewed and, in some cases, an MRI or CT scan may be necessary.
Proper treatment of a broken ankle will depend on where and how severe the break is, how stable the ankle is, and whether the bone is displaced (misaligned or separated) or non-displaced (broken yet still aligned properly).
Mild fractures (where the bone is non-displaced) may be treated by resting, icing, and elevating the ankle at first, followed by immobilization with a cast or walking boot. Pain and inflammation may be treated with acetaminophen. More severe or complicated fractures where bones or joints are displaced may require surgery.
Recovery time will also vary, and it may take 4-6 weeks or longer for a broken ankle to heal. Your podiatrist will most likely order progressive X-rays or stress tests to be taken in order to monitor the healing process.
Causes, Definition, and Embracing Life While Living With a Bunion

Bunions are a prevalent foot condition, bringing discomfort and challenges to daily life. These bony protrusions, medically known as hallux valgus, develop at the joint where the big toe meets the foot. They often occur from a combination of factors, including genetics, ill- fitting footwear, and structural anomalies in the foot. Defined by the outward deviation of the big toe and the subsequent misalignment of bones, bunions can cause pain, swelling, and difficulty in finding comfortable shoes. Living with bunions requires proactive measures. Choosing shoes that have ample toe space and arch support can help to reduce discomfort. Surgery may be needed for removal if the bunion is severe and affecting the other toes. If you have a bunion, it is strongly suggested that you are under the care of a podiatrist who can provide you with treatment options that are right for you.
If you are suffering from bunions, contact one of our podiatrists of William Street Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact one of our offices located in William Street in New York, NY, Forest Hills, NY, and Broadway in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Are You Suffering From Ingrown Toenails?
Risk Factors Associated With Foot Corns

Foot corns are hard, raised bumps that form due to excessive pressure or friction on the foot, leading to the deposit of keratin in the skin layers. Corns on the feet typically develop on or between the toes, below the toenail bed, or on the sole of the foot. Common causes include wearing tight or ill-fitting shoes, walking or running barefoot, and prolonged standing. The symptoms of foot corns include discomfort while walking or standing, pain, and in some cases, a burning sensation. To treat foot corns, it is essential to soften the skin and remove the thickened layers. This can be achieved through soaking the feet in warm water or using a pumice stone. Addressing the underlying cause is crucial to prevent recurrence, and this may involve changing shoe type or size. Certain risk factors can increase the likelihood of developing foot corns, such as diabetes, foot deformities, poor blood circulation, and overpronation or oversupination while walking. If over-the-counter remedies don't provide relief, it is suggested that you make an appointment with a podiatrist, which is especially important for anyone with diabetes or foot deformities.
If you have any concerns regarding your feet and ankles, contact one of our podiatrists of William Street Podiatry. Our doctors will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctors to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact one of our offices located in William Street in New York, NY, Forest Hills, NY, and Broadway in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns and Calluses
A corn is a lesion that forms in the skin of the foot, and it is typically circular in shape, small in size, and thick and rough in texture. A corn generally occurs as a result of repeated pressure on the skin; one example of this is the rubbing of a shoe against the skin. Corns differ from calluses in that their central cores are harder in texture.
A corn is a relatively common condition with a wide variety of treatment options. If a corn becomes overly uncomfortable or painful, consult with your podiatrist; he can determine the best method of treatment that is appropriate for you. Corns may return if the underlying cause of its development is not treated or removed. Avoid removing corns at home, as improper removal may cause infection.
A callus, similar to a corn, is an area of skin that has become thickened due to repeated pressure and rubbing. The rubbing causes the skin to create a layer of protective skin, which is the formed callus. Calluses can differ in size between people, and they can also become painful.
Multiple treatments are available for calluses. At-home treatment and removal should be avoided, as this can potentially lead to infection. Your podiatrist can best determine the cause of your calluses and suggest the treatment most appropriate for you.
Causes of Adult Acquired Flat Feet

Fallen arches is a condition that is termed posterior tibial tendon dysfunction, or PTTD. It also may be referred to as adult-acquired flat feet. Many people with flat feet suffer little or no problems. But others may experience pain if a tendon in the arch of the foot becomes inflamed, overstretched, or torn. The problem starts with the posterior tibial tendon, which begins in the leg, runs through the ankle, and connects to the bones in the bottom of the foot. When it is damaged, it can result in flat feet. This type of occurrence is far more prevalent in women, especially those between 40 and 60 years old. It is believed to be the result of overuse of the posterior tibial tendon. It is also common among runners and athletes who play high-impact sports. Other causes include diabetes, obesity, and high blood pressure. Symptoms include pain on the inside of the foot and ankle, accompanied by swelling, redness, and warmth. Symptoms usually spike after engaging in physical activity, such as jumping and running. For more information on this type of injury, it is suggested that you make an appointment with a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from William Street Podiatry. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in William Street in New York, NY, Forest Hills, NY, and Broadway in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
Seeking Relief for Plantar Fasciitis

Plantar fasciitis is a frequently encountered foot ailment that manifests as inflammation of the plantar fascia, the band of tissue connecting the heel bone to the toes. Repetitive stress on this area can lead to tiny tears, leading to severe heel discomfort, particularly during the initial steps in the morning or following extended periods of rest. This condition is commonly observed in athletes, runners, and individuals engaged in prolonged standing activities. A range of treatment options exists, including stretching exercises, orthotics, and physical therapy, all aimed at alleviating the symptoms and promoting healing. If you are grappling with this problem, it is suggested that you seek the expertise of a podiatrist to facilitate prompt recovery while preventing further deterioration.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from William Street Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in William Street in New York, NY, Forest Hills, NY, and Broadway in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.